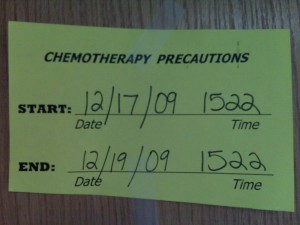
Well, it’s official: Colin’s I.V. chemo is done. He received a dose of vincristine Thursday afternoon at 3:22 pm. Chemotherapy will continue in a maintenance phase, but all taken orally and at much lower doses (and, for the most part, different drugs).
At St. Jude, there is a policy of having a “no mo’ chemo” party performed at a time and place of the patient’s choosing. Because we have been primarily inpatient, we are doing it in the second floor lobby on Monday at noon and will be bringing in a big stack of pizzas as well as inviting everybody who has helped us through this part of the journey.
One Silver Bead
There is also a bead program here that is mostly for older children and allows them to note various milestones and procedures, and for those who elect it, it replaces the tradition of toy collection. This can be stressful in its own right when one has a child who is too young to understand the concept of picking one toy out of a box filled with apt choices, and really the kids get enough toys as it is.
A silver bead marks the end of chemotherapy, and I look forward to collecting it. We have one bead for each course of chemo (now totaling four), each blood transfusion and so on. The bead collection starts with the child’s name and a St. Jude bead and goes from there.
In the first week, Colin earned the following beads: inpatient, isolation, blood transfusion, ICU, surgery, MRI, CT scan, x-ray x2, rehab x3 at least, chemotherapy, needle stick, dressing change (x3), and respiratory therapy. Much of this is fairly typical (imaging, rehab, and venous access) but some is not.
As Colin’s treatment progresses, it is interesting to see what beads he gets and, thus, mark what he is and is not needing along the way. For example, Colin gets blood products when his bone marrow suffers from the chemo and his blood production wanes. Over the past few days, as his counts have dropped, he has needed blood products on pretty much a daily basis.
Colin’s Adventures into Vampirism
The relationship between the effects of the chemotherapy and the blood is in some ways simple: the drugs target fast-dividing cells, including healthy bone marrow that produces various components found in blood. Most, though not all, chemo drugs are considered either “myelosuppressive” or “myeloablative.”
The first simply means that the bone marrow is suppressed and doesn’t produce as much as it should, and the second means that it essentially kills the bone marrow. In some forms of cancer like leukemia, these effects are independently useful and there is a clear utility to wiping out bone marrow in a patient whose bone marrow itself is diseased.
However, for brain tumors, the immunosuppression that occurs is an unfortuate and unnecessary side effect. In certain chemo regimens for brain tumors (not the one we pursued for Colin), the drugs that cause myeloablation may be particularly useful, and then the bone marrow needs to be repopulated. Again, this isn’t because the medical goal is directly related to the bone marrow but it coincidentally involves it.
In general, the treatment of solid tumor patients is quite different from that for leukemia patients, and the inpatient care is separated by these lines here. Furthermore, there is a special bone marrow transplant unit for patients who undergo myeloablative therapy that requires the replacement of the bone marrow, either through bone marrow stem cell transplant or bone marrow transplant. The brain tumor patients who need stem cells can use their own, which are harvested prior to treatment; other patients whose bone marrow stem cells are diseased have to get a transplant from somebody else. Both stay in the bone marrow transplant unit during this vulnerable time.
Interestingly, the expectations for hematology vary according to the type of disease being treated, and it is not uncommon for brain tumor patients to have a higher threshold for transfusions (in other words, they may get transfused earlier than the average leukemia patient). Generally speaking, brain tumor patients spend less time being neutropenic, and the duration of chemotherapy is much shorter.
In the past, Colin has experienced difficult-to-control bleeding when his platelets were near the range of 50,000 (the three zeroes are dropped in the lab results, so the shorthand is 50 even though it is actually in the thousands). This happened after the Target House photo shoot and we have always maintained him at that level. Furthermore, when he is neutropenic, his platelet levels tend to drop quickly, and transfusions seem to have little effect from one day to the next.
On Monday, Colin’s 4 a.m. labs showed that the transfusion of packed red blood cells had taken hold well so he was no longer close to debilitating anemia, he was at the brink of neutropenia (ANC=500), and his blood chemistries were fairly stable. On Tuesday, they did not order a repeat CBC, although I discussed this with his night nurse, who thought it would be a good idea.
Everything seemed fine on Tuesday, though he was showing up a fair amount of blood (mixed with sputum) in his trach. In the past, he has sometimes suffered from irritation in the trach from excessive deep suctioning or a particular incident that scraped the tissue in his trachea. In this case, since we have been extremely careful with suctioning, we chalked it up to a lot of dry coughing/gagging. It wasn’t the worst we had seen, though we were worried about making sure that he didn’t get aggressively suctioned.
Colin, Master of Surprises
Around dinnertime, I heard a big wet expulsion and went over to evaluate the damage. Instantly, I hit the call bell for help, since there was diarrhea all over the pad and I needed help to keep the lines clean. Then, I noticed something alarming that, upon closer inspection, got me to shut off his feeds and shoot out of the room.
I looked at our nurse, who was sitting at the nurse’s station. “Get a doctor, now!”
The line for the feeds attaches to the port that wends into Colin’s jejeunum. The port that goes directly into his stomach has been attached to a drainage back through the part of chemo that makes him nauseated, and this bag had been collecting normal yellow/green stomach juices for some time, with no trace of sloughing (the brown look of dried blood, but dilute) of the stomach or other mucosa.
However, the tubing leading into the jejeunum was filled with bright red blood. In times past, we have seen traces of blood here and there, and the litmus test of panic has always been, “Well, it’s not frank blood,” meaning an undiluted volume of fresh blood. This time, Colin failed that litmus test.
Despite the obvious and immediate concern over the appearance of blood from Colin’s G.I. tract, he otherwise seemed fine. This was reassuring, and we mounted the clean-up efforts to thankfully discover that he didn’t produce any blood in the diarrhea.
The process of getting a doctor (read: resident who is unfamiliar with Colin) in the room was longer than one would hope, and I emailed both of our doctors, knowing that somebody who actually knew Colin better needed to be on alert. Dr. DeWire issued her instructions based on information from the nurse.
The initial thought from the doctors, based on the chemo side effects, was that Colin was suffering from mucositis and we were seeing sloughing. However, Colin had not demonstrated any evidence of sloughing in the days that we had been draining his stomach contents and the problem was clearly localized somewhere between the pyloris (the opening at the bottom of the stomach) and the colon (given that there was no blood in the diarrhea, it couldn’t have originated from very close to the beloved endpoint).
The pressure from the big expulsion Colin had just produced probably pushed the blood up into the J-tube; because the feeds were set on a low flow rate that is, in reality, intermittent rather than constant, there was little positive pressure for the blood to push against.
The first matter was to run a CBC and determine whether Colin was simply unable to clot any injury that would cause bleeding, and we also needed to check the placement of the tubing to make sure it hasn’t somehow perforated the jejeunum.
When the lab work did finally come back, we found out that Colin’s platelets were at 19! A CBC earlier in the day would have revealed sub-50 levels and mandated a platelet transfusion, likely avoiding this drama in the first place. Normally, CBCs at this point of chemo are not run on a daily basis, yet I later realized, after arguing with our nurse about the previous day’s platelet level, that I was wrong because I had never looked at that particular number. Instead, I had the previous day’s level (78) stuck in my head.
There are three pieces of information particular to Colin that are important in this situation: (a) Colin’s platelets are kept above 50, as many but not all patients are; (b) Colin’s counts can plummet extremely quickly; (c) for him, platelets fade out very fast.
A CBC of 57 on Monday would certainly have warranted a CBC on Tuesday and do feel some responsibility for not pushing for it so. The situation that resulted was dramatic but not perilous, and it certainly does not suggest acute mismanagement. However, it underscores how individualized the details of medical care can be and how a specific experience or incident can color our future responses.
To wit, although all of the bleeding cleared up following Tuesday night’s transfusion and a repeat on Thursday morning. However, I noticed some bloody sputum in his trach on Thursday evening and asked to run labs. Within an hour, the mommy thermometer (kiss on the forehead) said that he was febrile100.6 by the mechanical variety, so they opted to expand a platelet count to a full CBC and blood cultures.
At 40, his platelets were not dangerously low and higher than the common “standard” of 35, so whatever invisible-to-me doctor was around opted not to transfuse him. After some pushback on my part (Defcon 2), fully anticipated by our nurse, he/she (I’m not suggesting that the doctor is a trannie but simply don’t know its actual gender) acceeded and ordered platelets. Defcon 3 would have involved a text message to Dr. DeWire, who explicitly told me to keep him above 50.
Again, the doctor’s response is neither surprising nor negligent. Protocols and standards exist so individual judgement does not need to play a role in every single decision. This has the ultimate effect of reducing error. However, when you have individuals who have enough information about the situation to arrive at a more informed and complete opinion, then the strict adherence to arbitrary guidelines is frustrating to say the least.
The Uninvited Education in Cancer
As Colin glides into neutropenia in the last cycle of I.V. chemo, it seems almost a shame for this vast education in his body and its reaction to various insults to go to waste. This is, presumably, his last descent into neutropenia (it is possible but not likely with either radiation or oral maintenance chemo) and the hematological problems that it creates.

This is the last time we will anxiously wait for his ANC to reappear and rise or have to react to a fever like he got bitten by a slavering hyena. We are now solidly past the misery of unrelenting vomiting, which was strangely less intense in the fourth round than it had been in the third.
Although the late effects of radiation tend to be much more serious than they are for chemotherapy of the kind that Colin just received, it is a relief to have slid past the (to him) unexplained, debilitating unpleasantness that he experienced with chemo.
The end of chemo is simultaneously momentous and anticlimactic, since the administration of the last, relatively innocuous, drug was itself one short moment within the continuum of Colin’s care. The drug is administered directly into the clave at the tip of the port access through a quick series of pushes and pulls on the syringe. All of the other chemo drugs he has had flow through the pump over the course of anywhere between one and 24 hours from a dangerous looking bag hanging on his I.V. pole. The bag arrives and departs in a yellow chemotherapy bag and any spills demand an immediate hazmat response.
Giving Colin vincristine is kind of a yawn, so it seems almost inappropriate to define the end of chemo at that moment. I felt more relief and accomplishment when the methotrexate and cisplatin had run, knowing that we were launching into that set of perils for the last time.
Even if through some twist of fate (unlikely at best) Colin were to get more chemo in the future, he will never get methotrexate, which has an extremely bad synergistic effect after radiation is done. Also, the cisplatin is too toxic a drug to use again if we don’t think it did much good this time.
One Shot at Chemo
Cancer cells are even more efficient than microbes in adapting to efforts to kill them, so the drugs become less effective. Even a drug that is effective one may lose its power over time, and one that fails to produce much if any result at all certainly won’t through repetition. More disconcerting, resistance to one drug within a class of drugs tends to confer resistance to other drugs within the class, since they rely on the same basic biological mechanism.
Combining different classes of drugs within the same therapeutic regimen increases the efficacy of the treatment, but to some extent it exhausts options. In the case of a cancer like ependymoma, which is only vaguely responsive to chemotherapy, there is no further role for aggressive chemotherapy. If anything, Colin would be one of the many brain tumor patients waiting for novel drugs and methods. Of course, we hope not to reach that juncture.
For now, we are in the hopeful place of seeking a complete cure for Colin’s cancer. Months ago, when a good resection seemed beyond our grasp and we were relying on a series of chemo and surgery to whittle away the tumor, it seemed like we were entering a long slog with many pitfalls along the way.
Today, we are less than two weeks away from the MRI that will tell us more about what is happening in Colin’s head and what next steps to take. Although we of course hope that the chemo has been effective, we are not relying on it to have melted the tumor remnant in order for it to be useful. I can’t imagine how this would feel if we were keeping a watchful eye on a much larger chunk of tumor that would be creating mass effect inside Colin’s head and possibly growing larger despite therapy.
One Step Closer
This is the home stretch toward a cure. Once Colin’s head is measurably free of tumor, the last step is radiation, and we will not know whether that is effective except through time and future scans. Although active treatment has given me the reassuring feeling that I am actually doing something, the watchful waiting game following the end of treatment looks better and better.
Even in the face of a stubborn tumor that comes back at some unknown point in time, once we are done with treatment, Colin will be feeling better, improving physically and neurologically and more able to enjoy being two-going-on-three. We will no longer have to fret over the details of managing immediate symptoms related to treatment, though I think the concerns about late effects (more likely radiation than chemo) will hover around us indefinitely.
Whether I like it or not, Colin has reached a milestone, or at least a milestone in the process that represents the “end of chemo.” Really, it’s hard to imagine it over until his ANC is above 500, which we will certainly broadcast with glee… next week(?).
We appreciate all of the support we have received during the course of Colin’s treatment, and we look forward to counting down the next milestones in our adventures in Memphis. We have every expectation that Colin will be home by Christmas, a symbolically important fact.
And we’ll be showing off that silver bead once Colin gets it.
We wish you all a Blessed Christmas together as a family!! And lets pray that the MRI on the 28th brings a celebration for the coming year.
The videos are great – he has made such progress with activity – it is wonderful. It is so nice to see a smile on his face.
Merry Christmas to all and Happy New Year
Keep fighting Colin!! We are all praying for you…
Well, as the Kung Fu Panda would say,
“LEGEND tells of a LEGENDary patient, whose ability to confound his doctors was the stuff of LEGEND…”
Seriously, it’s astounding to step back and think of what you all have been through in the past 6 months. Here’s to being home for Christmas, and all our best wishes go with you in the next phase of treatment.
Love, Paul, Caitlin & Matthias
PS, I loved your answer to Aidan when he demanded the truth about Santa.
Hey guys…we came home to IL yesterday and I found your website to keep in touch with you while we are apart. I know exactly what you are talking about when you say the vincristine is a bit of a yawn, it doesn’t feel like chemo! I pray little Colin does well with radiation. I know you are excited to get that going! I know I am. Do you know yet if there are any plans to remove the remaining tumor? I talked to Dr. Wright yesterday and I asked her if they have determined if the chemo had an effect on Maisie’s tumor and she said they did test on the tumor they removed and said it did. The molecular structure was different than what they removed in her first surgery! So I guess it works and it makes me feel like I didn’t put her through all that for nothing. Good luck with everything and hope you all have a merry christmas! We leave for FL January 4!!!
Hooray for the end of chemo. I can’t imagine what it’s like. In some ways you must all be thrilled at the prospect of going home. On the other hand, your life has been hospitals and treatments for so long that leaving it will almost seem strange. But adapting to home will be so wonderful.
Monday we’ll eat pizza and think about Colin’s steps towards victory!
Love, Diana
When I was a student at Uconn, I sang the role of Lord Mt. Arrarat in Gilbert and Sullivan’s Operetta Iolanthe. One of my most enjoyable pieces I was to recite: “Dark the dawn when day is neigh: hustle your horse and don’t say die…..if you go in, you’re sure to win….feint heart never won….”
GO! Go Colin, Tamiko, Ian, Aiden, Dr. Dewire, and all the Angels at St. Jude’s. Here’s to our Christmas Star at Memphis!!!!
Grandpa